Modulation of cardiac metabolism in heart failure
HTML: 1
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
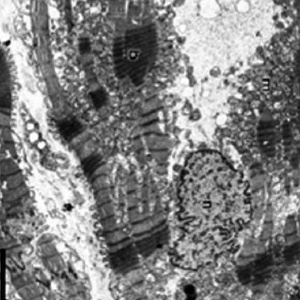
Authors
Heart failure is associated with altered cardiac metabolism, in part, due to maladaptive mechanisms, in part secondary to comorbidities such as diabetes and ischemic heart disease. The metabolic derangements taking place in heart failure are not limited to the cardiac myocytes but extend to skeletal muscles and the vasculature causing changes that contribute to the worsening of exercise capacity. Modulation of cardiac metabolism with partial inhibition of free fatty acid oxidation has been shown to be beneficial in patients with heart failure. At the present, the bulk of evidence for this class of drugs comes from trimetazidine. Newer compounds partially inhibiting free fatty acid oxidation or facilitating the electron transport on the mitochondrial cristae are in early phase of their clinical development.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.